方案详情
文
利用相位多普勒粒子干涉仪(PDI)对可插入肺内,在肺内部现场产生治疗效果的喷雾的装置Microjet™进行性能检测评价。
方案详情

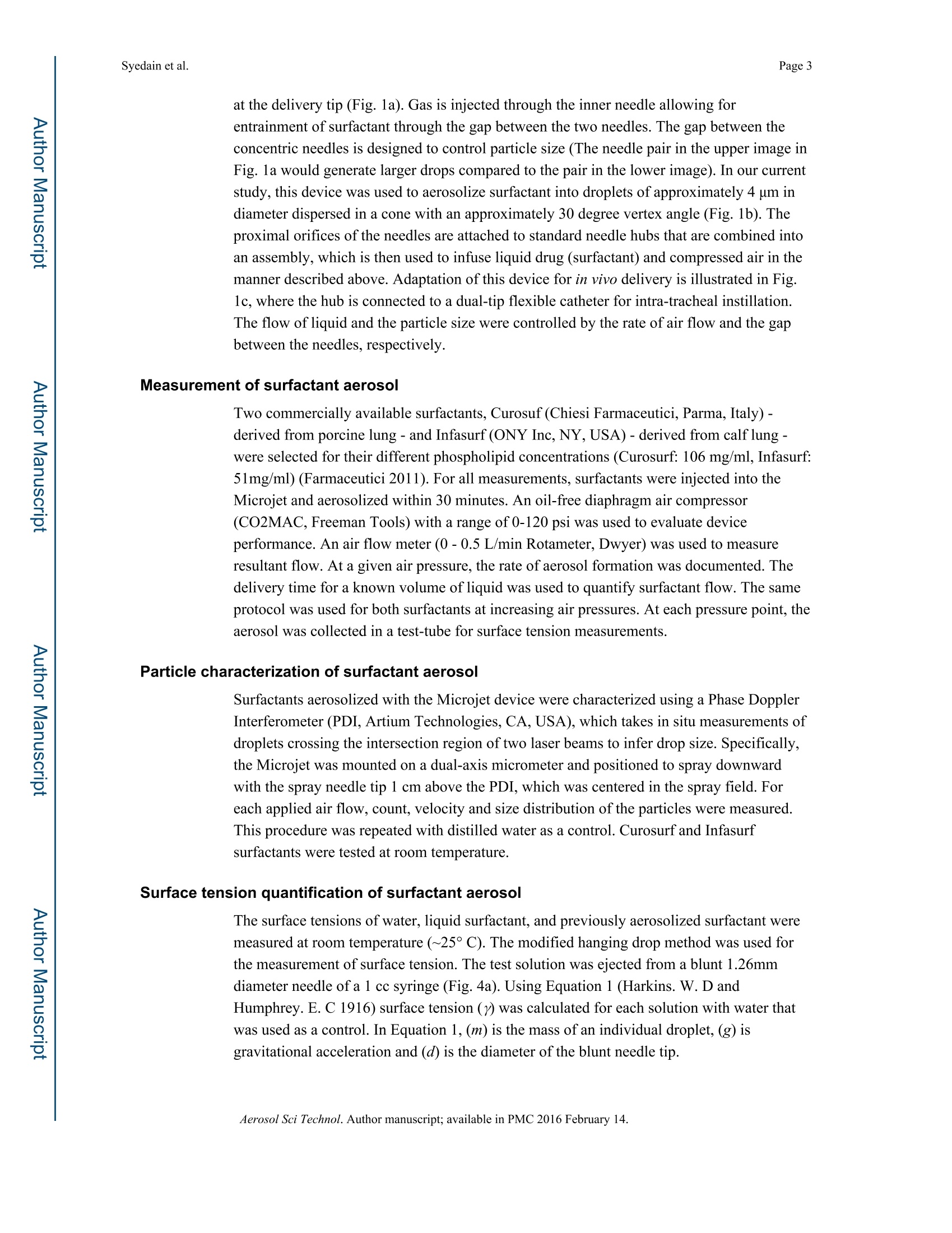
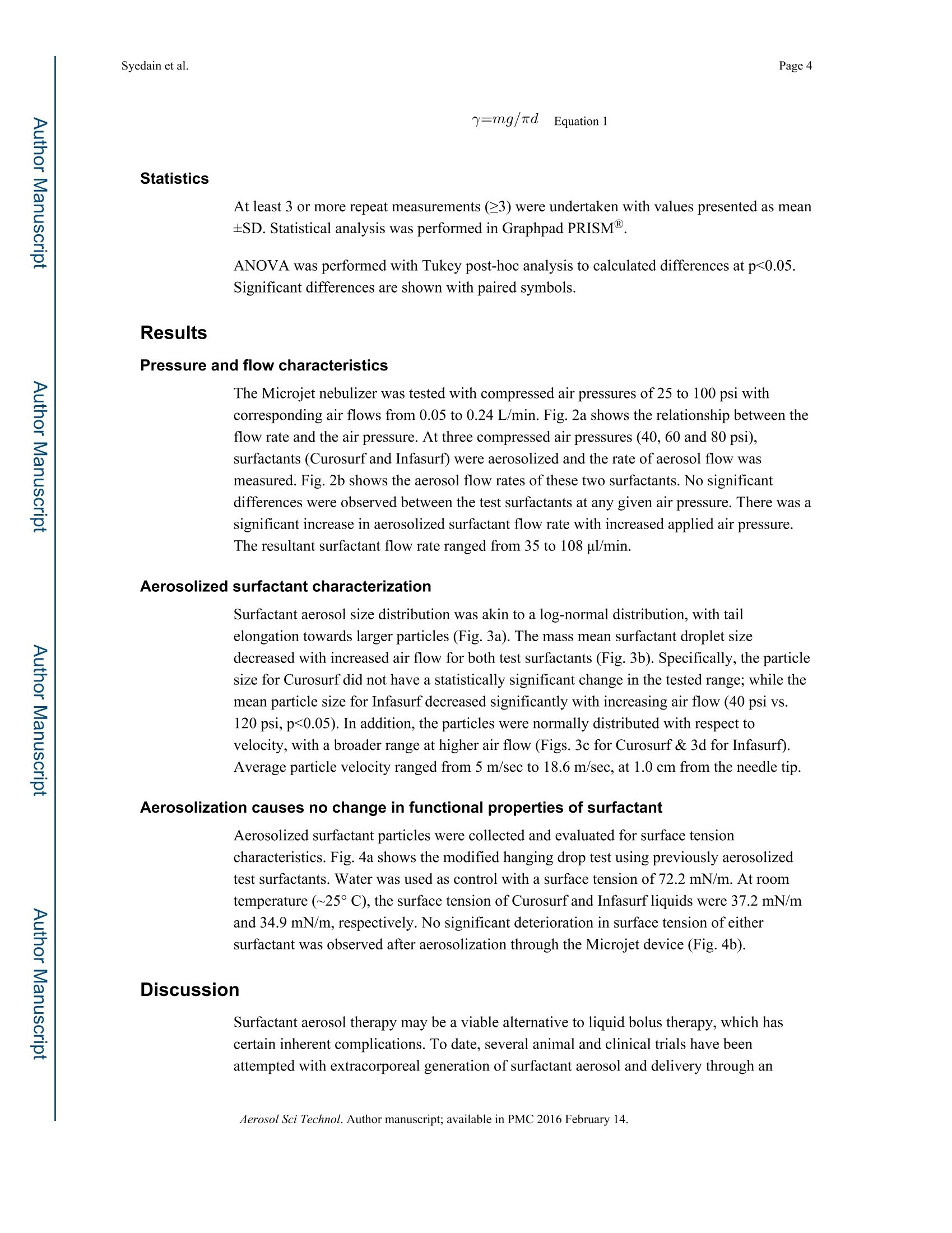
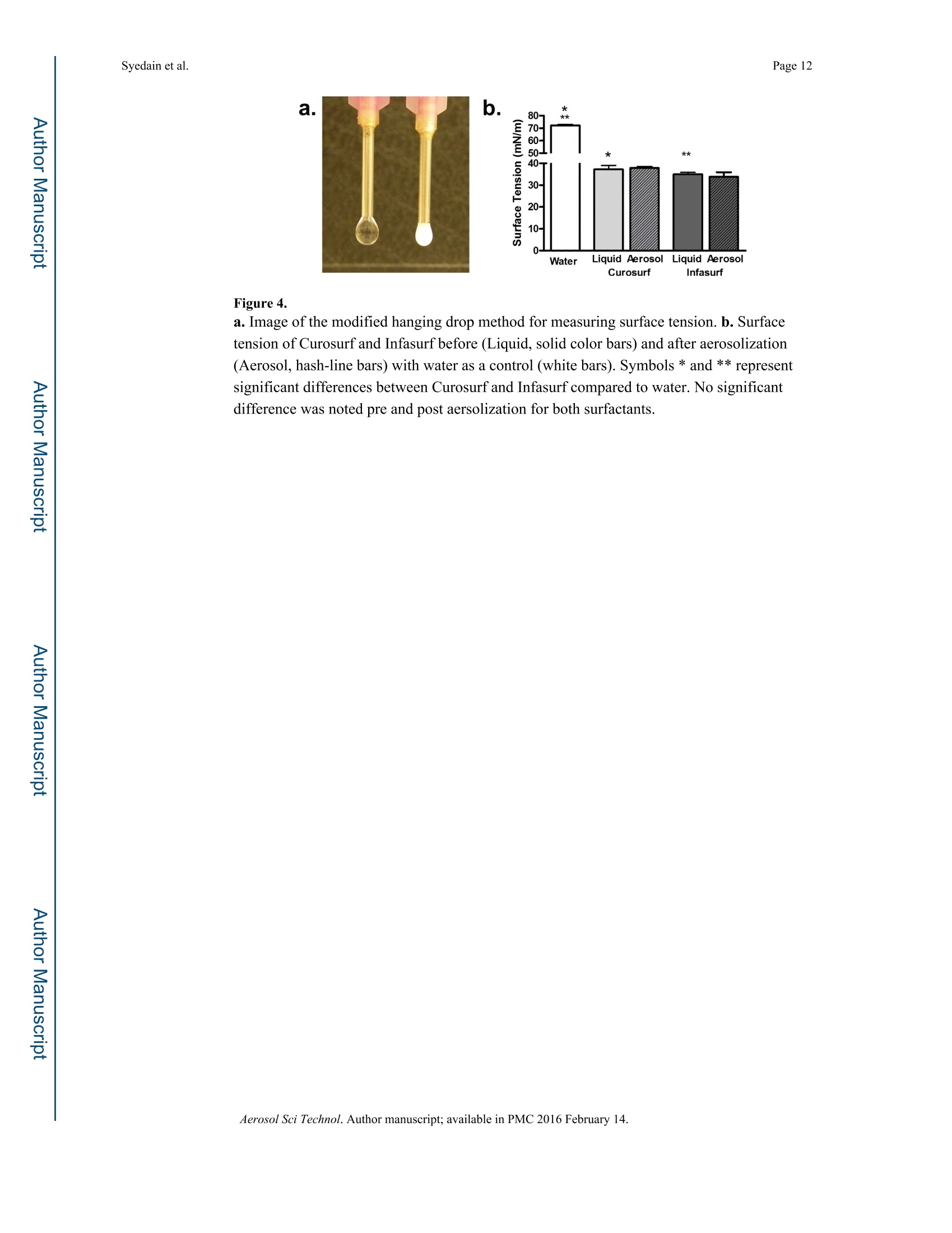
Author manuscriptAerosol Sci Technol. Author manuscript; available in PMC 2016 February 14.Published in final edited form as: Page 2Syedain et al. Disclosure Statement: HHS Public Access Aerosol Sci Technol. 2015 September 1;49(9): 747-752.doi:10.1080/02786826.2015.1067670. In Vitro Evaluation of a Device for Intra-Pulmonary AerosolGeneration and Delivery Zeeshan H. Syedain1.4, Amir A. Naqwi2, Myrna Dolovich3, and Arif Somani3,4 1Department of Biomedical Engineering, University of Minnesota,Minneapolis, Minnesota, USAMSP Corp, Shoreview, Minnesota, USA 3 Faculty of Health Sciences, McMaster University, Hamilton, Ontario, Canada 4Division of Critical Care, Department of Pediatrics, University of Minnesota, Minneapolis,Minnesota, USA Abstract For infants born with respiratory distress syndrome (RDS), liquid bolus delivery of surfactantadministered through an endotracheal tube is common practice. While this method is generallyeffective, complications such as transient hypoxia, hypercapnia, and altered cerebral blood flowmay occur. Aerosolized surfactant therapy has been explored as an alternative. Unfortunately, pastefforts have led to disappointing results as aerosols were generated outside the lungs withsignificant pharyngeal deposition and minimal intrapulmonary instillation. Dc寸ct A novel aerosol generator (MicrojetTM) is evaluated herein for intrapulmonary aerosol generationwithin an endotracheal tube and tested with Curosurf and Infasurf surfactants. Compared with other aerosol delivery devices, this process utilizes low air flow (range 0.01-0.2 L/min) that is ideal for limiting potential barotrauma to the premature newborn lung. The mass meandiameter (MMD) ofthe particles for both tested surfactants was less than 4 um, which is ideal forboth uniform and distal lung delivery. As an indicator of phospholipid function, surfactant surfacetension was measured before and after aerosol formation; with no significant difference.Moreover, this device has an outside diameter of <1mm, which permits insertion into anendotracheal tube (of even 2.0 mm). In the premature infant where intravenous access is eithertechnically challenging or difficult, aerosol drug delivery may provide an alternative route inpatient resuscitation, stabilization and care. Other potential applications of this type of deviceinclude the delivery of nutrients, antibiotics, and analgesics via the pulmonary route. ( Address correspondence to Arif Somani, Faculty of Health Sciences, McMaster University, HSC 3E20, 1280 M ain S treet West, H amilton, ON L 8 S 4K1, C an ada. somani@mcmaster.ca; or at Unive r sity of Minnesota, Ped i atric Crit i cal C a re 5 t h Floor EastBuilding, 8951G, 2450 Riverside Avenue , Minneapolis, MN 55455, USA. soman007@umn.edu. ) ( D r . Zeeshan S y edain was affiliated with Powerscope Inc. and the University of Minnesota at th e time of this research. Dr. Ami rN aqwi had ownership in Powerscope Inc. Drs Myr n a Dolovich and A r if Somani has no financ i al suppo r t from P owerscope. Dr. S omani h a s a collaborative grant submitted (R43 Sept. 2 0 13) with MSP Cor p . ) Introduction oact An estimated 1% of newborns in the US (i.e. about 40,000 neonates per year) developrespiratory distress syndrome (RDS) at birth (Rodriguez and Martin 1999). Such newbornsare normally given surfactant therapy in the delivery room, or shortly thereafter, in theneonatal intensive care unit. Treatment with exogenous surfactant improves gas exchangeand optimizes survival in newborn babies with RDS (Jobe 1993; Mercier and Soll 1993;Suresh and Soll 2002). Currently, surfactant is administered as a liquid bolus in the centralairways via an endotracheal tube followed by gradual distal pulmonary dissipation(Rodriguez and Martin 1999). Up to 19% of infants require repeat dosing due to RDSprogression (Verder et al. 1994). Although this has improved survival, current therapy mayresult in several complications. Specifically, rapid intratracheal administration of a largevolume of surfactant solution may cause transient hypoxia, hypercapnia, altered cerebralblood flow, and increase the incidence of intraventricular hemorrhage (Cowan et al. 1991;Gunkel and Banks 1993; Halliday and Robertson 1992).This is especially relevant in thevery premature infant and the critically unstable neonate. Therefore, it would be desirable todeliver surfactant using a gentler modality that more readily allows for an effective anduniform intra-pulmonary distribution. To this end, several animal experiments and clinicaltrials have been conducted to deliver surfactant as an aerosol. Results of these trials have notbeen promising and may preclude viable clinical application (Berggren et al. 2000; Fok et al.1998; Lewis et al. 1991; Lewis and McCaig 1993). For instance, in a study by Jorch et al.,only 10% of aerosolized surfactant was delivered in the pharyngeal tubing resulting in amodest gain in lung function (Jorch et al. 1997). More recently, the synthetic surfactantAerosurf has been clinically evaluated for aerosolized delivery with variable outcomes(Finer et al.2010). To our understanding, the above studies with natural surfactants were primarily limited bythe tested aerosol devices. Previous clinical work has been based on generating aerosolsoutside the lung with subsequent delivery into the lung using various breathing supportdevices (Mazela et al. 2007). These methods deliver less than 1% of surfactant to the lungs(Berggren et al. 2000; Fok et al. 1998). Further, these devices were designed to aerosolizeand deliver drugs using high air flow (of several liters/minute) into the lungs of adults underrelatively stable conditions (Berggren et al. 2000). Such required air flow would almostcertainly induce barotrauma in the neonatal or infant lung. A low flow device developed tomatch neonatal tidal volume and inspiratory phase with efficient surfactant delivery wouldbe an ideal solution to mitigate the above issues. Here, we present a novel device of narrowgauge (OD<1mm) to be inserted into an endotracheal tube that should allow intra-pulmonary aerosol generation and near complete drug delivery while maintaining low airpressure and flow. Materials and Method Catheter-based Aerosolization Device A catheter-based aerosolization device (MicrojetTM) developed by Powerscope Inc. (nowpart of MSP Corporation, MN, USA) was tested in this study. The proof-of-conceptexperiments were conducted with a prototype device that consists of two concentric needles ( Aerosol Sci T echnol. A uthor manuscript; available in P MC 2 0 16 February 14. ) at the delivery tip (Fig. 1a). Gas is injected through the inner needle allowing forentrainment of surfactant through the gap between the two needles. The gap between theconcentric needles is designed to control particle size (The needle pair in the upper image inFig. la would generate larger drops compared to the pair in the lower image). In our currentstudy, this device was used to aerosolize surfactant into droplets of approximately 4 um indiameter dispersed in a cone with an approximately 30 degree vertex angle (Fig. 1b). Theproximal orifices of the needles are attached to standard needle hubs that are combined intoan assembly, which is then used to infuse liquid drug (surfactant) and compressed air in themanner described above. Adaptation of this device for in vivo delivery is illustrated in Fig.lc, where the hub is connected to a dual-tip flexible catheter for intra-tracheal instillation.The flow of liquid and the particle size were controlled by the rate of air flow and the gapbetween the needles, respectively. Measurement of surfactant aerosol Two commercially available surfactants, Curosuf (Chiesi Farmaceutici, Parma, Italy)-derived from porcine lung- and Infasurf (ONY Inc, NY, USA) - derived from calf lung-were selected for their different phospholipid concentrations (Curosurf: 106 mg/ml, Infasurf:51mg/ml) (Farmaceutici 2011). For all measurements, surfactants were injected into theMicrojet and aerosolized within 30 minutes. An oil-free diaphragm air compressor(CO2MAC, Freeman Tools) with a range of 0-120 psi was used to evaluate deviceperformance. An air flow meter (0 - 0.5 L/min Rotameter, Dwyer) was used to measureresultant flow. At a given air pressure, the rate of aerosol formation was documented. Thedelivery time for a known volume of liquid was used to quantify surfactant flow. The sameprotocol was used for both surfactants at increasing air pressures. At each pressure point, theaerosol was collected in a test-tube for surface tension measurements. Particle characterization of surfactant aerosol Surfactants aerosolized with the Microjet device were characterized using a Phase DopplerInterferometer (PDI, Artium Technologies, CA, USA), which takes in situ measurements ofdroplets crossing the intersection region of two laser beams to infer drop size. Specifically,the Microjet was mounted on a dual-axis micrometer and positioned to spray downwardwith the spray needle tip 1 cm above the PDI, which was centered in the spray field. Foreach applied air flow, count, velocity and size distribution of the particles were measured.This procedure was repeated with distilled water as a control. Curosurf and Infasurfsurfactants were tested at room temperature. Surface tension quantification of surfactant aerosol cct The surface tensions of water, liquid surfactant, and previously aerosolized surfactant weremeasured at room temperature (~25°C). The modified hanging drop method was used forthe measurement of surface tension. The test solution was ejected from a blunt 1.26mmdiameter needle of a 1 cc syringe (Fig. 4a). Using Equation 1 (Harkins. W. D andHumphrey. E. C 1916) surface tension ()) was calculated for each solution with water thatwas used as a control. In Equation1, (m) is the mass of an individual droplet, (g) isgravitational acceleration and (d) is the diameter of the blunt needle tip. ( Aerosol Sci T echnol. A uthor manuscript; available in P MC 2 0 16 February 14. ) y=mg/rd Equation 1 Statistics At least 3 or more repeat measurements (3) were undertaken with values presented as mean±SD. Statistical analysis was performed in Graphpad PRISM. ANOVA was performed with Tukey post-hoc analysis to calculated differences at p<0.05.Significant differences are shown with paired symbols. Results Pressure and flow characteristics The Microjet nebulizer was tested with compressed air pressures of 25 to 100 psi withcorresponding air flows from 0.05 to 0.24 L/min. Fig. 2a shows the relationship between theflow rate and the air pressure. At three compressed air pressures (40, 60 and 80 psi),surfactants (Curosurf and Infasurf) were aerosolized and the rate of aerosol flow wasmeasured. Fig. 2b shows the aerosol flow rates of these two surfactants. No significantdifferences were observed between the test surfactants at any given air pressure.There was asignificant increase in aerosolized surfactant flow rate with increased applied air pressure.The resultant surfactant flow rate ranged from 35 to 108 pl/min. Aerosolized surfactant characterization Surfactant aerosol size distribution was akin to a log-normal distribution, with tailelongation towards larger particles (Fig.3a). The mass mean surfactant droplet sizedecreased with increased air flow for both test surfactants (Fig. 3b). Specifically, the particlesize for Curosurf did not have a statistically significant change in the tested range; while themean particle size for Infasurf decreased significantly with increasing air flow (40 psi vs.120 psi, p<0.05). In addition, the particles were normally distributed with respect tovelocity, with a broader range at higher air flow (Figs. 3c for Curosurf & 3d for Infasurf).Average particle velocity ranged from 5 m/sec to 18.6 m/sec, at 1.0 cm from the needle tip. Aerosolization causes no change in functional properties of surfactant Aerosolized surfactant particles were collected and evaluated for surface tensioncharacteristics.Fig. 4a shows the modified hanging drop test using previously aerosolizedtest surfactants. Water was used as control with a surface tension of 72.2 mN/m. At roomtemperature(~25°C), the surface tension of Curosurf and Infasurf liquids were 37.2 mN/mand 34.9 mN/m, respectively. No significant deterioration in surface tension of eithersurfactant was observed after aerosolization through the Microjet device (Fig. 4b). cDiscussionct Surfactant aerosol therapy may be a viable alternative to liquid bolus therapy, which hascertain inherent complications. To date, several animal and clinical trials have beenattempted with extracorporeal generation of surfactant aerosol and delivery through an ( Aerosol Sci T echnol. A uthor manuscript; available in P MC 2 0 16 February 14. ) endotracheal tube. These studies have resulted in limited success (Berggren et al. 2000; Finer et al. 2010; Fok et al. 1998; Jorch et al. 1997; Lewis et al. 1991; Sun et al. 2009).Although an animal model showed promise, Berggren et al. found no significant benefit in aclinical trial of neonatal respiratory distress syndrome (Berggren et al. 2000).Moreover,actual pulmonary deposition could not be measured accurately. Factors that maycompromise clinical utility include aerosol loss via deposition in the pharyngeal space,which curtails an extracorporeal aerosol generation approach. Variable compliance indiseased lung segments may also limit or alter distal pulmonary aerosol delivery. Anobstacle in translating aerosol therapy to the neonatal patients has been a lack of anappropriate device (Mazela and Polin 2011). For instance, the majority of aerosol nebulizerdevices are designed to operate with an air flow of 5-8 L/min, which may be a suitable airflow for an adult with a lung tidal volume of 500 mL and a high inspiratory to expiratoryratio (I:E of3:5). However, these devices cannot be safely applied to an infant with anaverage tidal volume of 50 mL and an I:E ratio of 1:5 (Dolovich 2002). Further,commercially available devices have high environment and pharyngeal losses as shown byFok et al, where more than 99% of surfactant was lost in the device chamber and ventilatortubing (Fok et al.1998).Similarly, commercial nebulizers designed for adults demonstratelow efficiency when applied to neonates (Amirav et al. 2003; Amirav et al. 2002; Tal et al.1996). More recently, a vibrating mesh device with low flow has been tested using Aerosurf,a synthetic surfactant developed by Discovery Lab (not currently approved by the FDA)(Finer et al. 2010). It remains to be seen if a vibrating mesh nebulizer can be applied to a wide array of surfactant products without clogging the mesh. Given the need for a low flow aerosol generator, the Microjet device was evaluated. TheMicrojet is a narrow bore (<1 mm OD) device with concentric needle tips that allows for airshearing of liquid particles to generate a fine aerosol. The small size of the air needle (33gauge) allows the device to generate a high air velocity without requiring a high air flowwhich is especially attractive for neonatal application. Moreover, the PDI flow meter systemmeasured an almost complete decline in air velocity within 2 cm from the needle tip. Byeliminating the impactor dome found in a majority of commercially available jet nebulizers,this device also avoids potential impaction damage to large molecules like surfactants,proteins and plasmids (unpublished data). In this study, aerosol testing was performed withCurosurf (porcine) and Infasurf (bovine) surfactants, which were chosen for their widevariation in total phospholipid concentrations (Farmaceutici 2011). Microjet was evaluated at operating air pressures up to 80 psi with a corresponding air flowof<0.2 L/min, yielding a surfactant aerosol flow of 0.11 ml/min. Based on these conditions,1 ml of surfactant can be delivered in less than 10 minutes. For the pre-term neonate, a doseof 100 mg/kg would be required (Mazela et al. 2007). Based on a 100 mg/ml concentrationof Curosurf and a 50 mg/ml concentration of Infasurf, total therapy would require 10-20minutes. Due to its lack of dead space and intra-tracheal aerosol generation for drugdelivery, this device may even enable lower drug dosing. Further studies are required forclinical feasibility. Theoretically, low air flow complements pressure support ventilation andcontinuous positive pressure support, without exceeding normal neonatal tidal volumes.Moreover, it may be coordinated to match inspiratory cycles on a ventilator. Resultant ( Aerosol Sci T echnol. A uthor manuscript; available in P MC 2 0 16 February 14. ) surfactant particles had a mass mean diameter (MMD) of<4 um. This is attractive, as priorresearch has shown uniform lung distribution with particles of <4 um (Asgharian et al. 2003;Raabe et al. 1988). Another catheter-style aerosol device was tested by Murgia et al. using Curosurf (Murgia etal. 2011). The air flow with this catheter was greater than 1 L/min and aerosol particle sizeranged from 8 to 30 um. Although this catheter design also allows for endotracheal delivery,the greater air velocity may cause epithelial trauma; and with larger aerosol particlesgenerated, may compromise distal lung delivery (Raabe et al. 1988). Of benefit, Microjethas an air flow of less than 0.2 L/min, but it is unclear what air velocity is safe to minimizeepithelial damage during intra-tracheal surfactant aerosol generation. Drug formulation may also affect surfactant delivery (Fok et al. 1998). At varied airpressures, Infasurf (with a lower phospholipid concentration), but not Curosurf (with ahigher phospholipid concentration), yielded variable particle sizes (see Fig.3). Fok et al,showed that a synthetic surfactant (Exosurf, GlaxoSmithKline,UK) with a low phospholipidconcentration had higher deposition in an animal model than a natural surfactant (Survanta,Abbot Pharma, US) with a higher phospholipid concentration. Both Curosurf and Infasurfhad velocity distribution profiles that changed with increased air pressure. The ability toadjust particle size and velocity for a given drug or formulation, may allow for targeted lungdistribution. In conclusion, this study tested Microjet, an aerosol device that operates at low air flow,generates small aerosol particles, and maintains tested surfactant surface tensions. Thisdevice may overcome challenges faced by current nebulizer technology (Fok et al.1998).Future preclinical and clinical studies will be required to determine if this provides a safeand efficacious treatment option for RDS and other lung diseases. The potential of intra-pulmonary drug aerosol generation and delivery is an especially attractive clinicalapplication in premature and neonatal patients and warrants further development and testing. Acknowledgement The authors would like to thank the University of Minnesota Fairview Children's Hospital pharmacy for providingCurosurf and Infasurf and Zehraa Cheaib with manuscript assistance. Research reported in this publication was supported by the National Center for Advancing Translational Sciences ofthe National Institutes of Health Award Number UL1TR000114 and NIH SBIR 5R44EY016229-05.The content issolely the responsibility of the authors and does not necessarily represent the official views of the NationalInstitutes of Health. References Amirav I, Balanov I, Gorenberg M, Groshar D, Luder AS. Nebuliser hood compared to mask inwheezy infants: aerosol therapy without tears! Archives of disease in childhood. 2003; 88:719-723.[PubMed: 128761731 Amirav I, Balanov I, Gorenberg M, Luder AS, Newhouse MT, Groshar D. Beta-agonist aerosoldistribution in respiratory syncytial virus bronchiolitis in infants. Journal of nuclear medicine :official publication, Society of Nuclear Medicine. 2002; 43:487-491. Asgharian B, Kelly JT, Tewksbury EW. Respiratory deposition and inhalability of monodisperseaerosols in Long-Evans rats. Toxicol Sci. 2003;71:104-111.[PubMed: 12520080] ( Aerosol Sci T echnol. A uthor manuscript; available in P MC 2 0 16 February 14. ) ( Berggren E, Liljedahl M , Winbladh B, Andreasson B, C urstedt T,Robertson B, Schollin J. Pilot study of nebulized surfactant therapy for neonatal respiratory distress syndrome. Acta Paediatr. 2000;89:460-464.[PubMed: 10830460] ) Cowan F, Whitelaw A, Wertheim D, Silverman M. Cerebral blood flow velocity changes after rapid administration of surfactant. Archives of disease in childhood. 1991; 66:1105-1109.[PubMed: 1750756] Dolovich MB. Assessing nebulizer performance. Respiratory care. 2002; 47:1290-1301. discussion 1301-1294.[PubMed: 12425744] Farmaceutici C. CUROSURFR (poractant alfa) Intratracheal Suspension information. 2011 Finer NN, Merritt TA, Bernstein G, Job L, Mazela J, Segal R. An open label, pilot study of Aerosurf(R) combined with nCPAP to prevent RDS in preterm neonates. J Aerosol Med Pulm Drug Deliv. 2010; 23:303-309.[PubMed: 20455772] Fok TF, al-Essa M, Dolovich M, Rasid F, Kirpalani H. Nebulisation of surfactants in an animal model of neonatal respiratory distress. Arch Dis Child Fetal Neonatal Ed. 1998; 78:F3-9. [PubMed: 95368321 Gunkel JH, Banks PL. Surfactant therapy and intracranial hemorrhage: review of the literature and results of new analyses. Pediatrics. 1993; 92:775-786.[PubMed: 8233736] ( Halliday H, Robertson B. Cerebral blood flow velocity changes after rapid administration of surfactant . Archives of disease in childhood.1992;67:470. [PubMed: 1586196] ) ( Harkins WD, Humphrey EC. The Drop Weight Met h od for the Determination of Surface Tension. J. Am. C hem Soc. 1916;38:228-2 3 6. ) ( Jobe AH. Pulmonary surfactant therapy. The New England journal of medicine . 1993;328:861-868.[PubMed: 8441430] ) ( Jorch G , H artl H, R oth B, Kribs A, Gortner L , Schaible T, H e nnecke KH, Poets C. Sur f actant aerosol treatment of respiratory distress syndrome in spontaneously breathing premature infants. PediatrPulmonol. 1997;24:222-224 . [PubMed: 9330420] ) ( Lewis JF, I kegami M, J o be AH, Ta b or B. Aerosolized sur f actant treatment of preterm lambs. Journalof applied physiolog y . 1991;70:869-876.[PubMed:2022579] ) ( Lewis JF, M cCaig L. Aerosolized ve r sus in s tilled exogenous surfactant in a nonuniform pattern of lung injury. Am Rev R espir Dis. 1993; 148:1 1 87-11 9 3.[PubMed: 8239152] ) ( Mazela J, Merritt TA, Finer NN. Aerosolized surfactants. Curr Opin Pediatr. 2007 ; 19:155- 1 62. [PubMed: 174967581 ) ( Mazela J, P olin RA. Aerosol delivery to ventilated newborn infants: historical challenges and new directions. Eur J Pediatr. 2011;170:4 3 3-444.[PubMed:20878336] ) Mercier CE,Soll RF. Clinical trials of natural surfactant extract in respiratory distress syndrome.Clinics in perinatology. 1993; 20:711-735.[PubMed: 8131364] Murgia X, Gastiasoro E, Mielgo V, Alvarez-Diaz F, Lafuente H, Valls-i-Soler A, Gomez-Solaetxe MA, Larrabe JL, Rey-Santano C. Surfactant and perfluorocarbon aerosolization by means of inhalation catheters for the treatment of respiratory distress syndrome: an in vitro study. J Aerosol Med Pulm Drug Deliv.2011;24:81-87.[PubMed: 21410324] ( Raabe OG, Al-Bayati MA, Tea g ue SV, R asolt A. Regional deposition of inhaled monodisperse coarse and f ine aerosol particles in small laboratory animals. Ann. Occup. Hyg. 1988;32:53-63. ) ( Rodriguez R J , Martin R J . Exogenous surfactant therapy in newborns. Respir Care Clin N Am. 1999 ; 5:595-616. [PubMed: 10565883] ) Sun Y, Yang R, Zhong JG, Fang F, Jiang JJ, Liu MY, Lu J. Aerosolised surfactant generated by a novel noninvasive apparatus reduced acute lung injury in rats. Crit Care. 2009;13:R31.[PubMed: 192579071 Suresh GK, Soll RF. Lung surfactants for neonatal respiratory distress syndrome: animal-derived or synthetic agents? Paediatric drugs. 2002; 4:485-492.[PubMed: 12126452] Tal A, Golan H, Grauer N, Aviram M, Albin D, Quastel MR. Deposition pattern of radiolabeledsalbutamol inhaled from a metered-dose inhaler by means of a spacer with mask in young childrenwith airway obstruction. J Pediatr. 1996; 128:479-484.[PubMed: 8618180] ( Aerosol Sci T echnol. A uthor manuscript; available in P MC 2 0 16 February 14. ) Verder H, Robertson B, Greisen G, Ebbesen F, Albertsen P, Lundstrom K, Jacobsen T. Surfactanttherapy and nasal continuous positive airway pressure for newborns with respiratory distresssyndrome.Danish-Swedish Multicenter Study Group. The New England journal of medicine.1994;331:1051-1055. [PubMed:8090164] ( Aerosol Sci T echnol. A uthor manuscript; available in P MC 2 0 16 February 14. ) a. b. 400 pm oca 400 um t i. Drc. ug 0.57mm 0.21 mm Gas ii. -Luer-fittings Steel hub cct Figure 1. Design of needle-based aerosol generator (Microjet) a. End-on view of needle tip showingconcentric needles with inner needle for air flow and outer cavity for liquid flow. Twodifferent outer needle sizes are shown with a gap of 200 um and 100 um b. Image of aerosolspray from the tip of the needle at 40 psi air pressure.c. Schematic of catheter based device(diameter 1.5mm) with needle tip and flexible plastic tubing to supply air and liquid. ( Aerosol Sci T echnol. A uthor manuscript; available in P MC 2 0 16 February 14. ) Figure 2. a. Air flow as a function of applied back pressure using a compressor pump. b. Flow rate ofCurosurf and Infasurf as a function of applied back pressure. Symbol * and ** representsignificant differences among all three applied pressures at p<0.05. ( Aerosol Sci T echnol. A uthor manuscript; available in P MC 2 0 16 February 14. ) Figure 3. Aerosol characterization of surfactant using a Phase Doppler Interferometer (Artium Techologies, CA, USA) a. Aerosol particle size distribution profile for Curosurf. b. AverageMMD as a function of air pressure. Symbol * indicates significant difference between pairedgroups (P<0.05).c. Velocity profile of Curosurf aerosol. d. Velocity profile of Infasurfaerosol at 40, 60 and 80 psi back-pressure. Dc cct ( Aerosol Sci T echnol. A uthor manuscript; available in P MC 2 0 16 February 14. ) Syedain et al. Figure 4. a. Image of the modified hanging drop method for measuring surface tension. b. Surfacetension of Curosurf and Infasurf before (Liquid, solid color bars) and after aerosolization(Aerosol, hash-line bars) with water as a control (white bars). Symbols * and ** representsignificant differences between Curosurf and Infasurf compared to water. No significantdifference was noted pre and post aersolization for both surfactants. Dc cct ( Aerosol Sci T echnol. A uthor manuscript; available in P MC 2 0 16 February 14. ) For infants born with respiratory distress syndrome (RDS), liquid bolus delivery of surfactant administered through an endotracheal tube is common practice. While this method is generally effective, complications such as transient hypoxia, hypercapnia, and altered cerebral blood flow may occur. Aerosolized surfactant therapy has been explored as an alternative. Unfortunately, past efforts have led to disappointing results as aerosols were generated outside the lungs with significant pharyngeal deposition and minimal intrapulmonary instillation.A novel aerosol generator (Microjet™) is evaluated herein for intrapulmonary aerosol generation within an endotracheal tube and tested with Curosurf and Infasurf surfactants.Compared with other aerosol delivery devices, this process utilizes low air flow (range 0.01-0.2 L/min) that is ideal for limiting potential barotrauma to the premature newborn lung. The mass mean diameter (MMD) of the particles for both tested surfactants was less than 4 μm, which is ideal for both uniform and distal lung delivery. As an indicator of phospholipid function, surfactant surface tension was measured before and after aerosol formation; with no significant difference. Moreover, this device has an outside diameter of <1mm, which permits insertion into an endotracheal tube (of even 2.0 mm). In the premature infant where intravenous access is either technically challenging or difficult, aerosol drug delivery may provide an alternative route in patient resuscitation, stabilization and care. Other potential applications of this type of device include the delivery of nutrients, antibiotics, and analgesics via the pulmonary route.
确定






还剩10页未读,是否继续阅读?
北京欧兰科技发展有限公司为您提供《烟雾粒子中微液滴粒径和速度检测方案(激光干涉仪)》,该方案主要用于其他中微液滴粒径和速度检测,参考标准--,《烟雾粒子中微液滴粒径和速度检测方案(激光干涉仪)》用到的仪器有激光相位多普勒干涉仪LDV,PDI,PDPA,PDA
相关方案
更多
该厂商其他方案
更多